However, while owning a pulse oximeter is a powerful step
toward preventive healthcare, many people struggle with one critical question:
What do these numbers actually mean, and when should you see a doctor? A
reading of 93%, 90%, or even 88% can trigger panic in some families, while
others dangerously ignore warning signs because the patient “looks okay.” This
confusion can lead to both unnecessary hospital visits and life-threatening
delays in medical care.
One of the most dangerous realities of modern respiratory
illness is silent hypoxia, a condition where oxygen levels drop dangerously low
without causing obvious breathlessness. During the COVID-19 pandemic, thousands
of patients reached hospitals too late because they felt only mild fatigue
while their oxygen levels had already fallen into critical ranges. Even today,
post-viral lung damage, heart disease, air pollution, and seasonal infections
continue to cause silent oxygen drops in high-risk individuals.
At Aarogyaa Bharat, we regularly guide families on how to
interpret pulse oximeter readings correctly and take timely medical action.
This comprehensive guide explains in maximum depth how to understand SpO₂
numbers, what ranges are safe or dangerous, how symptoms change the urgency
level, common false alarms, high-risk patient categories, when to monitor at
home, and exactly when a doctor visit becomes non-negotiable.
What a Pulse Oximeter Actually Measures
A pulse oximeter measures two vital parameters: blood oxygen
saturation (SpO₂) and pulse rate. SpO₂ represents the percentage of hemoglobin
in the blood that is carrying oxygen. Since oxygen fuels every organ in the
body, even small declines in oxygen levels can create widespread health
consequences if not addressed in time.
The device works using a technology called
photoplethysmography. It shines red and infrared light through the fingertip
and analyzes how much light is absorbed by oxygenated and deoxygenated
hemoglobin. This calculation allows the device to estimate oxygen saturation
within seconds, without needles, pain, or blood samples.
Pulse rate, the second reading, reflects how fast the heart
is beating to circulate oxygen throughout the body. When oxygen levels drop,
the heart often compensates by beating faster, which is why rising pulse rates
alongside falling SpO₂ values are especially concerning.
Modern pulse oximeters also display waveform graphs,
perfusion indexes, and trend data, helping users track oxygen fluctuations over
time. These additional features are especially valuable for chronic patients
and post-COVID survivors monitoring long-term recovery.
Understanding Normal, Borderline, and Dangerous SpO₂
Ranges
Interpreting SpO₂ values correctly is the foundation of safe
home monitoring. While exact thresholds may vary slightly between individuals,
the following general ranges are widely accepted in clinical practice.
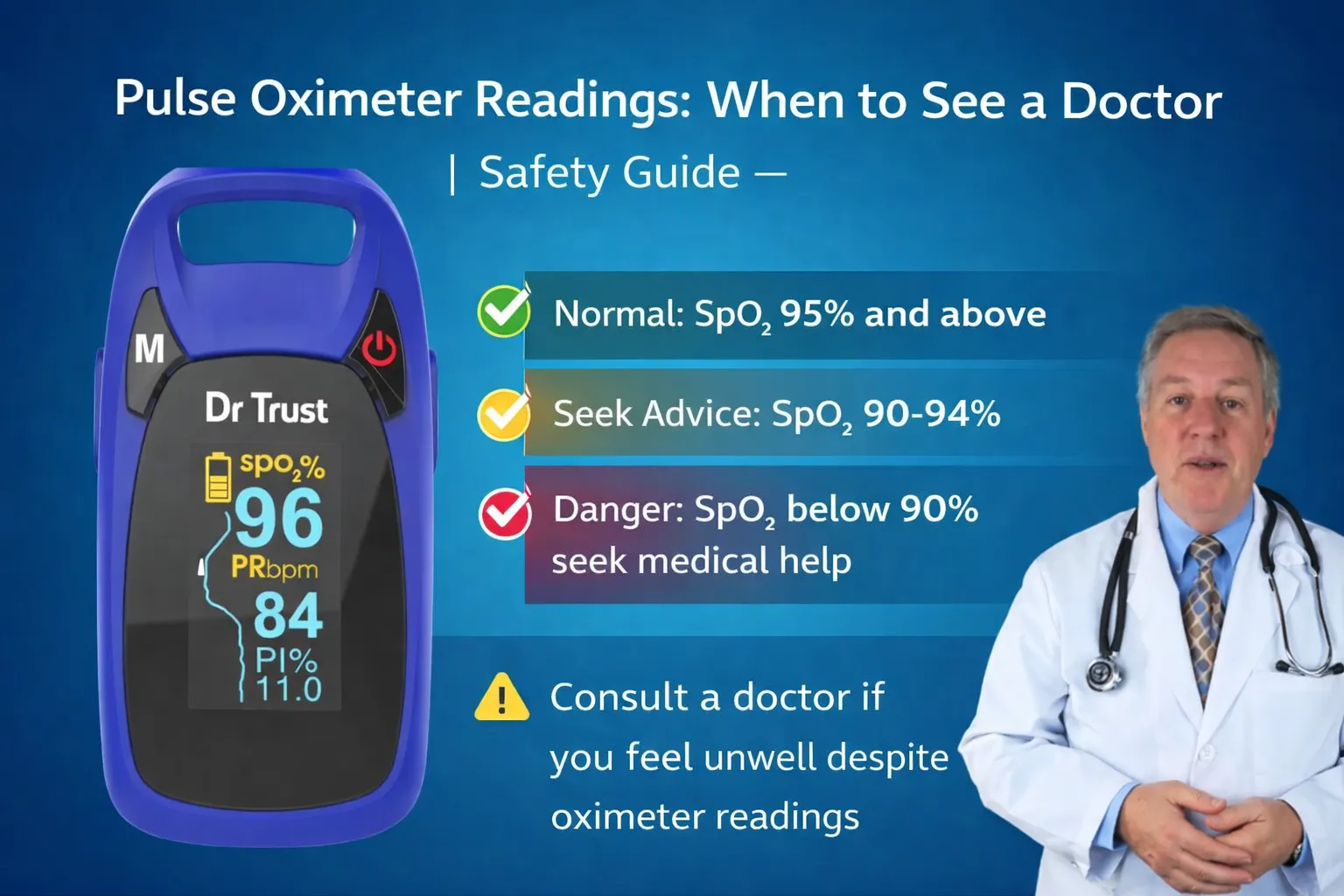
An SpO₂ reading between 95% and 100% is considered normal
for healthy adults at sea level. This range indicates that the lungs are
effectively oxygenating the blood and that the heart is circulating oxygen
efficiently to vital organs.
Readings between 90% and 94% fall into a borderline zone
known as mild hypoxemia. While not immediately life-threatening, this range
requires close monitoring, especially if the patient has underlying lung or
heart disease. Persistent readings in this range often signal early respiratory
compromise and should not be ignored.
Readings between 85% and 89% indicate moderate hypoxemia and
require medical evaluation. At this level, organs such as the brain and heart
begin to receive insufficient oxygen, increasing the risk of confusion,
arrhythmias, and respiratory failure.
Readings below 85% are considered severe hypoxemia and
constitute a medical emergency. At these levels, immediate oxygen therapy and
hospital care are necessary to prevent organ damage or death.
For patients with chronic lung disease, doctors may
establish individualized target ranges slightly lower than standard norms.
However, any sudden drop from baseline values even if still above 90% is a red
flag requiring medical consultation.
When a Pulse Oximeter Reading Is an Emergency
Some oxygen levels demand immediate medical attention
regardless of how the patient appears. If the pulse oximeter consistently shows
SpO₂ below 90%, it is no longer safe to manage the situation at home without
medical supervision.
Readings below 88% are particularly dangerous because they
indicate that the lungs are failing to supply adequate oxygen to vital organs.
At this stage, patients are at high risk of respiratory failure, heart
arrhythmias, and sudden collapse.
If SpO₂ drops below 85%, emergency services should be
contacted immediately. Do not attempt home remedies, breathing exercises, or
delayed monitoring at this stage. Oxygen therapy and hospital evaluation are
urgently required.
Another emergency scenario is a rapid downward trend. If
oxygen levels fall from 96% to 92% to 88% within a short time span, this rapid
deterioration is more dangerous than a stable low reading and demands urgent
medical care.
Any low oxygen reading accompanied by severe breathlessness,
bluish lips, chest pain, confusion, or fainting should be treated as a medical
emergency, even if the numeric value seems only moderately low.
When Borderline Readings Still Require a Doctor Visit
Many families mistakenly assume that oxygen levels between
90% and 94% are “safe enough” and delay seeking medical advice. While this
range is not immediately life-threatening, it often represents the early stages
of respiratory deterioration.
Persistent readings in this borderline zone over several
hours or days suggest that the lungs are under strain and may worsen without
treatment. This is particularly dangerous for elderly individuals, asthma
patients, post-COVID survivors, and people with heart disease.
If SpO₂ remains below 94% for more than 24 hours, a doctor
consultation is strongly recommended, even if symptoms are mild. Early
intervention at this stage can prevent hospitalization and serious
complications.
Borderline readings combined with symptoms such as fatigue,
headache, chest tightness, mild breathlessness, or night-time oxygen drops
should always trigger a medical evaluation.
For chronic lung disease patients, a drop of more than 3-4%
from their usual baseline even if still above 90% is a significant warning sign
requiring prompt medical advice.
Symptoms That Make Any Reading More Dangerous
Oxygen numbers never exist in isolation. Symptoms
dramatically change how urgently a doctor should be consulted, even when
readings appear moderately normal.
If a patient experiences shortness of breath at rest,
difficulty speaking full sentences, or visible chest retractions, immediate
medical attention is required regardless of SpO₂ value.
Chest pain or pressure, especially in heart patients,
combined with low or borderline oxygen levels may indicate a cardiac emergency
and requires urgent hospital evaluation.
Confusion, drowsiness, agitation, or sudden personality
changes are signs that the brain is not receiving enough oxygen. These
neurological symptoms often appear before oxygen numbers fall into critical
ranges.
Bluish lips or fingertips (cyanosis) are late signs of
severe hypoxia and demand emergency care even if the pulse oximeter reading
seems borderline.
Rapid heart rate (above 110-120 bpm) combined with falling
SpO₂ values indicates that the heart is struggling to compensate for oxygen
deficiency and requires urgent medical evaluation.
High-Risk Groups Who Should See a Doctor Earlier
Certain individuals should seek medical advice at higher
SpO₂ thresholds because their bodies cannot tolerate low oxygen levels safely.
Elderly individuals often develop serious complications at
oxygen levels that younger adults may tolerate. For seniors, any reading below
94% should prompt a doctor consultation.
Asthma, COPD, and chronic lung disease patients should seek
medical care when SpO₂ falls below 92% or drops significantly from baseline,
even if symptoms are mild.
Post-COVID survivors frequently experience delayed lung
complications. Any sustained drop below 94% or worsening trend should be
evaluated by a doctor.
Heart disease patients face increased cardiac strain when
oxygen levels fall. Even borderline readings in the low 90s can trigger
arrhythmias or heart failure exacerbations.
Children should be monitored closely because they
deteriorate faster than adults. SpO₂ below 94% in children should prompt
medical consultation, and below 90% requires urgent care.
When Home Monitoring Is Enough (and When It Is Not)
Home monitoring is appropriate when SpO₂ remains above 94%,
symptoms are mild, and readings are stable over time. In such cases, rest,
hydration, medication adherence, and daily monitoring may be sufficient.
However, home monitoring is not enough when readings fall
below 92%, symptoms worsen, or oxygen levels show a downward trend. In these
scenarios, delaying medical care can result in sudden deterioration.
Pulse oximeters are screening tools, not diagnostic devices.
They help identify problems early but cannot replace professional medical
evaluation when danger thresholds are crossed.
Common False Alarms and How to Avoid Them
Not all low readings reflect true hypoxia. Cold fingers
reduce blood flow and can cause falsely low readings. Always warm hands before
measurement.
Nail polish, artificial nails, and dirty sensors interfere
with light absorption and distort readings. Remove nail cosmetics and clean the
device regularly.
Movement during measurement produces erratic numbers. Keep
the hand still and wait 10-15 seconds for the reading to stabilize.
Low battery levels and poor-quality devices can produce
inaccurate results. Always use a certified medical-grade pulse oximeter for
reliable monitoring.
Quick Decision Guide Table
|
SpO₂
Reading |
Symptoms
Present? |
What to Do |
|
95%-100% |
No |
Normal,
continue daily monitoring |
|
90%-94% |
No |
Monitor
closely, consult doctor if persistent |
|
90%-94% |
Yes |
See a doctor
within 24 hours |
|
85%-89% |
Any |
Seek medical
evaluation urgently |
|
Below 85% |
Any |
Call emergency services immediately |
Conclusion
A pulse oximeter is one of the most powerful tools for early
detection of respiratory and cardiac problems at home. However, its true
life-saving potential lies not just in owning the device, but in knowing when
to act on its readings.
Understanding safe oxygen ranges, recognizing dangerous
trends, accounting for symptoms, and identifying high-risk situations can mean
the difference between timely treatment and a life-threatening emergency.
Silent hypoxia, borderline oxygen levels, and rapid deterioration often go
unnoticed until it is too late unless daily monitoring is combined with
informed medical decision-making.
At Aarogyaa Bharat, we are committed to helping families use
pulse oximeters not just as gadgets, but as true preventive healthcare tools.
Whether you are monitoring elderly parents, managing chronic illness,
recovering from COVID-19, or simply prioritizing daily wellness, our expert
guidance ensures you take the right action at the right time.
If you ever feel uncertain about your pulse oximeter
readings, Aarogyaa Bharat is always here to help you interpret results, choose
the right monitoring device, and connect with professional care when it matters
most.